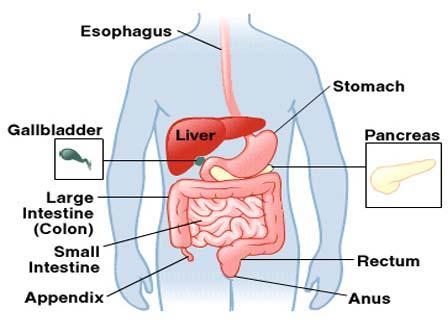
Ulcerative colitis is a chronic inflammation of the large intestine (colon). The colon is the part of the digestive system where waste material is stored. The rectum is the end of the colon adjacent to the anus. In patients with ulcerative colitis, ulcers and inflammation of the inner lining of the colon lead to symptoms of abdominal pain, diarrhea, and rectal bleeding.
Ulcerative colitis is closely related to another condition of inflammation of the intestines called Crohn’s disease. Together, they are frequently referred to as Inflammatory bowel disease (IBD). Ulcerative colitis and Crohn’s diseases are chronic conditions that can last years to decades. Men and women are affected equally. They most commonly begin during adolescence and early adulthood, but they also can begin during childhood and later in life.
It is found worldwide, but is most common in the United States, England, and northern Europe. It is especially common in people of Jewish descent. Ulcerative colitis is rarely seen in Eastern Europe, Asia, and South America, and is rare in the black population. For unknown reasons, an increased frequency of this condition has been recently observed in developing nations.
Causes Of Ulcerative Colitis
The causes of ulcerative colitis and Crohn’s Disease are unknown. To date, there has been no convincing evidence that these two diseases are caused by infection. Neither disease is contagious.
Ulcerative colitis and Crohn’s disease are caused by abnormal activation of the immune system in the intestines. The immune system is composed of immune cells and the proteins that these cells produce. These cells and proteins serve to defend the body against harmful bacteria, viruses, fungi, and other foreign invaders. Activation of the immune system causes inflammation within the tissues where the activation occurs. (Inflammation is, in fact, an important mechanism of defense used by the immune system.) Normally, the immune system is activated only when the body is exposed to harmful invaders. In patients with Crohn’s disease and ulcerative colitis, however, the immune system is abnormally and chronically activated in the absence of any known invader. The continued abnormal activation of the immune systems causes chronic inflammation and ulceration. The susceptibility to abnormal activation of the immune system is genetically inherited. First-degree relatives (brothers, sisters, children, and parents) of patients with IBD are thus more likely to develop these diseases.
Symptoms of Ulcerative Colitis
Common symptoms of ulcerative colitis include rectal bleeding and diarrhea, but there is a wide range of symptoms among patients with this disease. Variability of symptoms reflects differences in the extent of disease (i.e., the amount of the colon and rectum that are inflamed) and the intensity of inflammation. Generally, patients with inflammation confined to the rectum and a short segment of the colon adjacent to the rectum have milder symptoms and a better prognosis than patients with more widespread inflammation of the colon. The different types of ulcerative colitis are classified according to the location and the extent of inflammation :
1. Ulcerative Proctitis : refers to inflammation that is limited to the rectum. In many patients with ulcerative proctitis, mild intermittent rectal bleeding may be the only symptom. Other patients with more severe rectal inflammation may, in addition, experience rectal pain, urgency (sudden feeling of having to defecate and a need to rush to the bathroom for fear of soiling), and tenesmus (ineffective, painful urge to move one’s bowels).
2. Proctosigmoiditis involves inflammation of the rectum and the sigmoid colon (a short segment of the colon contiguous to the rectum). Symptoms of proctosigmoiditis, like that of proctitis, include rectal bleeding, urgency, and tenesmus. Some patients with proctosigmoiditis also develop bloody diarrhea and cramps.
3. Left-sided colitis involves inflammation that starts at the rectum and extends up the left colon (sigmoid colon and the descending colon). Symptoms of left-sided colitis include bloody diarrhea, abdominal cramps, weight loss, and left-sided abdominal pain.
4. Pancolitis or universal colitis refers to inflammation affecting the entire colon (right colon, left colon, transverse colon and the rectum). Symptoms of pancolitis include bloody diarrhea, abdominal pain and cramps, weight loss, fatigue, fever, and night sweats. Some patients with pancolitis have low-grade inflammation and mild symptoms that respond readily to medications. Generally, however, patients with pancolitis suffer more severe disease and are more difficult to treat than those with more limited forms of ulcerative colitis.
5. Fulminant colitis is a rare but severe form of pancolitis. Patients with fulminant colitis are extremely ill with dehydration, severe abdominal pain, protracted diarrhea with bleeding, and even shock. They are at risk of developing toxic megacolon (marked dilatation of the colon due to severe inflammation) and colon rupture (perforation). Patients with fulminant colitis and toxic megacolon are treated in the hospital with potent intravenous medications. Unless they respond to treatment promptly, surgical removal of the diseased colon is necessary to prevent colon rupture.
While the intensity of colon inflammation in ulcerative colitis waxes and wanes over time, the location and the extent of disease in a patient generally stays constant. Therefore, when a patient with ulcerative proctitis develops a relapse of his disease, the inflammation usually is confined to the rectum. Nevertheless, a small number of patients (less than 10%) with ulcerative proctitis or proctosigmoiditis can later develop more extensive colitis. Thus, patients who initially only have ulcerative proctitis can later develop left-sided colitis or even pancolitis.
Diagnosis of Ulcerative Colitis :-
The diagnosis of ulcerative colitis is suggested by the symptoms of abdominal pain, rectal bleeding, and diarrhea. Stool specimens are collected for analysis to exclude infection and parasites, since these conditions can cause colitis that mimics ulcerative colitis. Blood tests may showan anemia and an elevated white blood cell count or sedimentation rate (commonly referred to as sed rate). An elevated white blood cell count and sed rate both reflect ongoing inflammation in the colon. Confirmation of ulcerative colitis requires a test to visualize the large intestine. Flexible tubes inserted through the rectum (sigmoidoscopes and colonoscopes) permit direct visualization of the inside of the colon to establish the diagnosis and to measure the extent of the colitis. Small tissue samples (biopsies) can be obtained during the procedure to determine the severity of the colitis. Knowledge of the extent and severity of the colitis is important in choosing among treatment options. A barium enema x-ray may also indicate the diagnosis of ulcerative colitis. During a barium enema, a chalky substance is administered into the rectum and injected into the colon. Barium is radiopaque and can outline the colon on x-ray pictures. A barium enema is less accurate and useful than direct visualization techniques in the diagnosis of ulcerative colitis.
Complications of Ulcerative Colitis :-
Patients with ulcerative colitis limited to the rectum (proctitis) or colitis limited to the end of the left colon (proctosigmoiditis) usually do quite well. Brief periodic treatments using oral medications or enemas may be sufficient. Serious complications are rare in these patients. In those with more extensive disease, blood loss from the inflamed intestines can lead to anemia, and may require treatment with iron supplements or even blood transfusions. Rarely, the colon can acutely dilate to a large size when the inflammation becomes very severe. This condition is called toxic megacolon. Patients with toxic megacolon are extremely ill with fever, abdominal pain and distention, dehydration, and malnutrition. Unless the patient improves rapidly with medication, surgery is usually necessary to prevent colon rupture.
Colon Cancer is a recognized complication of chronic ulcerative colitis. The risk for cancer begins to rise significantly after eight to ten years of colitis. The risk of a patient with ulcerative colitis developing colon cancer is also related to the location and the extent of their disease. Patients with only ulcerative proctitis probably do not have increased colon cancer risk compared to the general population. Among patients with active pancolitis of 10 years or longer, their risk of colon cancer is 10-20 times that of the general population. In patients with chronic left-sided colitis, the risk of colon cancer is increased but not as high as in patients with chronic pancolitis.
Since these cancers have a more favorable outcome when caught at an earlier stage, yearly colon examinations may be recommended after eight years of known extensive disease. During these examinations, samples of tissue (biopsies) can be taken to search for precancerous changes in the lining cells of the colon. When precancerous changes are found, removal of the colon may be necessary to prevent colon cancer.
Complications of ulcerative colitis can involve other parts of the body. Ten percent of the patients can develop inflammation of the joints (arthritis). Some patients have low back pain due to arthritis of the sacroiliac joints. Rarely, patients may develop painful, red, skin nodules (erythema nodosum). Yet others can have painful, red eyes (uveitis, episcleritis). Because these particular complications can risk permanent vision impairment, eye pain or redness are symptoms that require a physician’s evaluation. Diseases of the liver and bile ducts may also be associated with ulcerative colitis. For example, in rare patients with a condition called sclerosing cholangitis, repeated infections and inflammation in the bile ducts can lead to recurrent fever, yellowing of skin (Jaundice, cirrhosis), and the need for a liver transplant.
Ayurveda Approach :-
There are many medicines, which works on Ulcerative Colitis, herbs try to stronger the Immune System of the Body and relieves the symptoms of the disease.
